My 2.5-year journey with translocation renal cell carcinoma
April 30, 2024
This is a guest post by Dawn Dyson, 37, who was diagnosed with translocation renal cell carcinoma in 2022. Dawn…
Read More
We rounded up a few research highlights from the 2024 ASCO Genitourinary Cancers Symposium (ASCO GU), held recently in San Francisco, California.
Adjuvant immunotherapy improved survival after nephrectomy and could be new standard of care
Researchers are touting a potential new standard of care following surgery for clear cell renal cell carcinoma (RCC) patients with an intermediate- to high-risk of recurrence who have had a nephrectomy.
Adjuvant treatment with pembrolizumab – meaning it is given after surgery – resulted in a 38% reduced risk of death and improved disease-free and overall survival compared with placebo after nearly 5 years of follow up. These results from the randomized phase 3 Keynote-564 trial are the first to show clinically meaningful, statistically significant survival benefit for adjuvant therapy, results “51 years in the making” according to primary researcher Dr. Toni Choueiri of the Dana-Farber Cancer Institute, who presented the results at the 2024 ASCO GU meeting.
The standard of care following nephrectomy has been observation and, should a patient have disease recurrence, they might be treated with systemic therapy, additional surgery, or radiation. Adjuvant treatment with pembrolizumab may be an additional and potentially superior option for post-operative patients at risk of recurrence. The reported benefits held true across several subgroups included in the trial, although the results are not generalizable to people with non-clear cell RCC, since they were not included in the study. [2024 ASCO GU, Abstract LBA359] Read more.
Longest follow-up results continue to support combo nivolumab plus ipilimumab immunotherapy
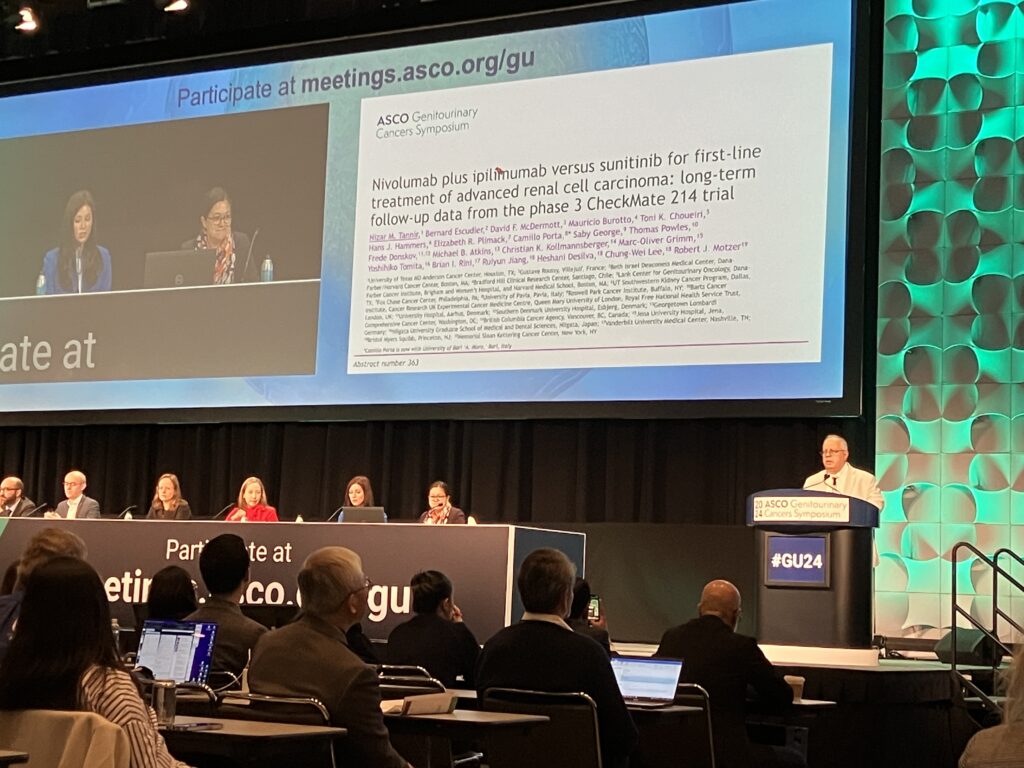
Nivolumab plus ipilimumab is still superior to sunitinib for treating advanced RCC in the first-line setting, according to the longest follow-up of a phase 3 trial – over 8 years of follow-up – of a combination immunotherapy regimen. Sunitinib is an earlier generation kidney cancer treatment, a kinase inhibitor that prevents excessive cell growth while immunotherapies use the body’s immune system to target and kill cancer cells. Overall survival results remained stable over that time, progression-free survival was more likely, treatment response was better including more complete responses, and long-term safety was manageable in the combination immunotherapy group compared with the sunitinib group. Lead investigator of the CheckMate 214 trial, Dr. Nizar Tannir of MD Anderson Cancer Center and emeritus member of the Kidney Cancer Association’s Medical Steering Committee, said the results continued supporting the use of nivolumab plus ipilimumab as standard-of-care for kidney cancer patients in this setting. [2024 ASCO GU, Abstract 363] Read more.
Injectable nivolumab was as good as infusion, could improve quality of life
Administering the immunotherapy nivolumab by an injection under the skin (subcutaneously) was as effective as administering nivolumab directly into a vein via an infusion, which is the current administration technique. This finding from the CheckMate67T study of patients with advanced kidney cancer means that there are more options for how to receive nivolumab if that is the treatment they are on. The main benefit of an injection is less time spent traveling for and receiving treatment. An infusion takes about 30 minutes on average and is done in a hospital or clinic setting. An injection could potentially be taken locally and the injection time was less than 5 minutes, although an extended injection might not be appealing to some patients. Side effects were also similar between the subcutaneous and intravenous nivolumab groups in this randomized phase 3 trial of nearly 500 patients. The amount of nivolumab used was higher in the subcutaneous group versus the intravenous group because more drug was needed to reach the same level of efficacy. This may have implications for cost of treatment. [2024 ASCO GU, Abstract LBA360]
Patient advocates involved in developing improved mRCC quality of life assessment tool
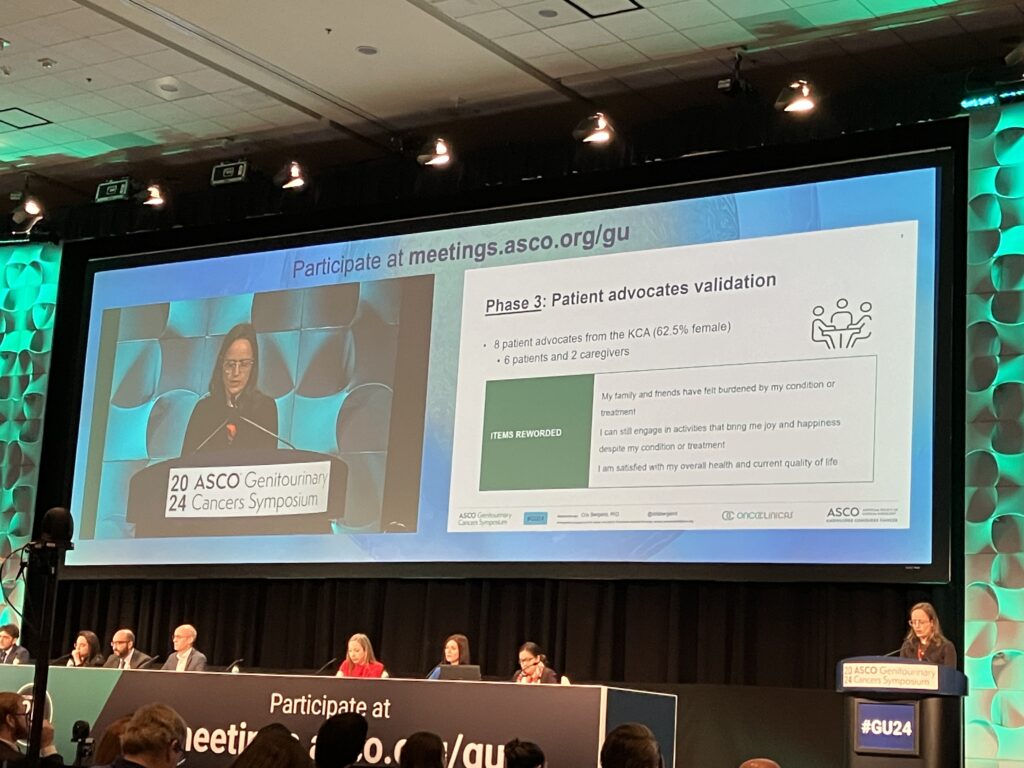
An ongoing project to develop a clearer, more relevant tool to assess health-related quality of life (HRQOL) in metastatic kidney cancer patients could help improve our understanding of the impacts of kidney cancer on patients and families. Results from pivotal kidney cancer trials over the years that have used various and less refined HRQOL tools, some of which are 30 years old – can be challenging to interpret, said lead investigator Dr. Cristiane Bergerot, a kidney cancer expert at Oncoclinicas in Brazil and a 2021 Kidney Cancer Association grant recipient for an earlier stage of this research. Bergerot began by surveying 117 patients about 54 questionnaire items from existing HRQOL surveys, 27% (15 items) of which were deemed relevant. Among those, patients suggested leaving some items unchanged, such as “I have a lack of energy” or “I have pain”, some were reworded, and two items – “My family has been affected by my condition or treatment” and “I am capable of care for myself independently” – were added. Bergerot and her team used both medical experts and a group of 8 patient advocates (6 patients, 2 caregivers) to validate a new questionnaire and ensure it was clear and relevant to the kidney cancer experience. Advocate inputs included suggestions like rewording to include groups like “friends” or to clarify some statements. Additional validation for the revised tool is in progress in upcoming trials to do a retrospective analysis and a primary assessment. [2024 ASCO GU, Abstract 365]
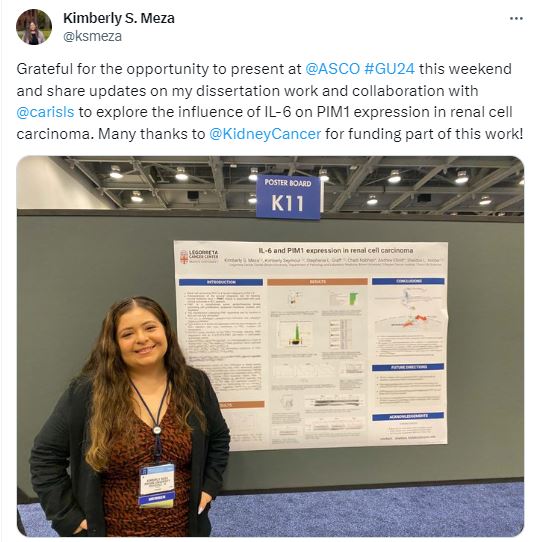
Potential new target for existing kidney cancer therapies
A different cellular pathway that contributes to poor outcomes in clear cell RCC could be a therapeutic target for which existing kidney cancer treatments are effective. Researchers at Brown University led by Dr. Sheldon Holder, a 2022 KCA grant recipient whose research led to this poster presentation, presented research showing that the kinase PIM1 is overexpressed in clear cell RCC tumors and the downstream effects mean people with the diagnosis have poorer outcomes regardless of what treatment they receive. Future work to better understand PIM1 expression and the associated cellular pathways could help refine what anti-cancer strategies might be effective in the context of RCC. [2024 ASCO GU, Poster K11]