
Understanding Subcutaneous Injections for Kidney Cancer Immunotherapy
This blog post has been funded by an educational grant from Bristol Myers Squibb.
Immunotherapy has become an important treatment option for many people living with kidney cancer. While these medicines have traditionally been given through an IV infusion, some immunotherapies are now also available as a subcutaneous injection. Understanding how these options compare can help patients have more informed conversations with their care team about what may work best for them. Below are answers to common questions about subcutaneous injections and IV infusions.
1. What is a subcutaneous injection?

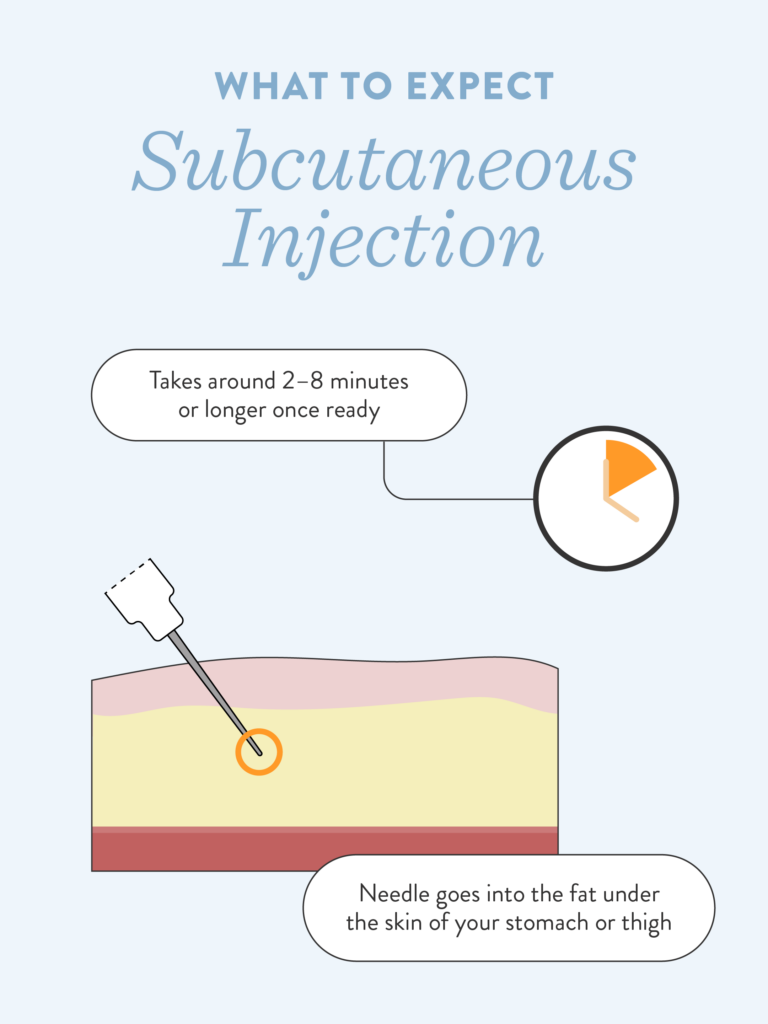
A subcutaneous injection delivers medicine into a layer of fat just beneath the skin, typically in the stomach or thigh. This method is commonly used for medications like insulin and is now approved for certain kidney cancer immunotherapies.
2. How is this different from an IV infusion?
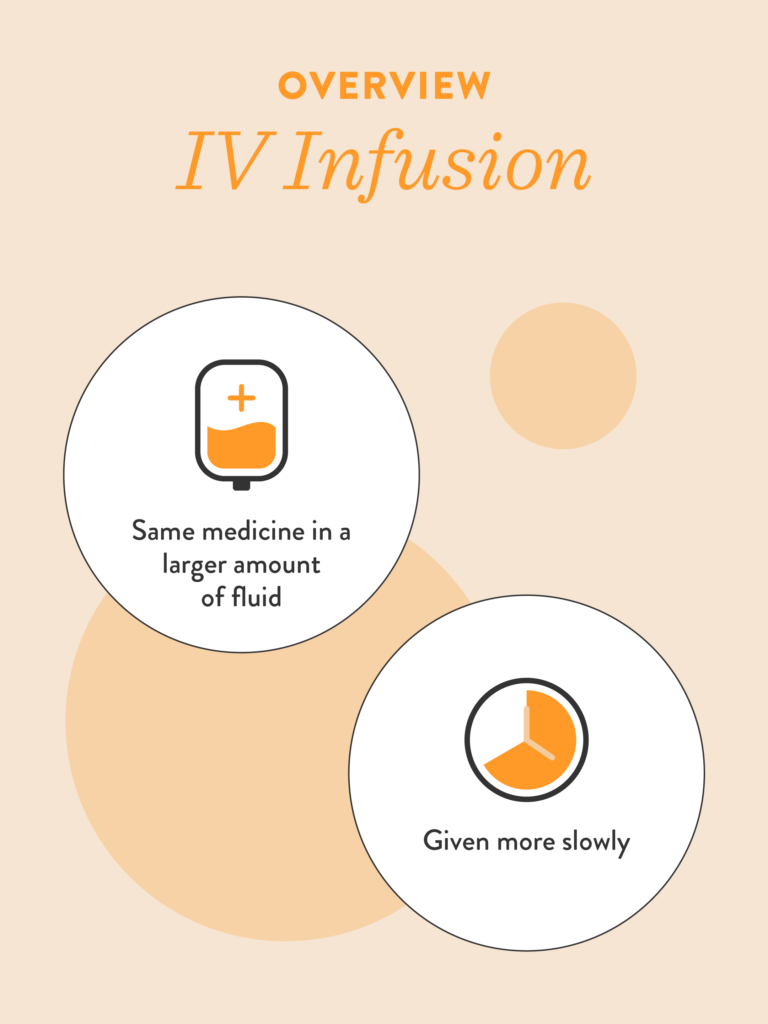
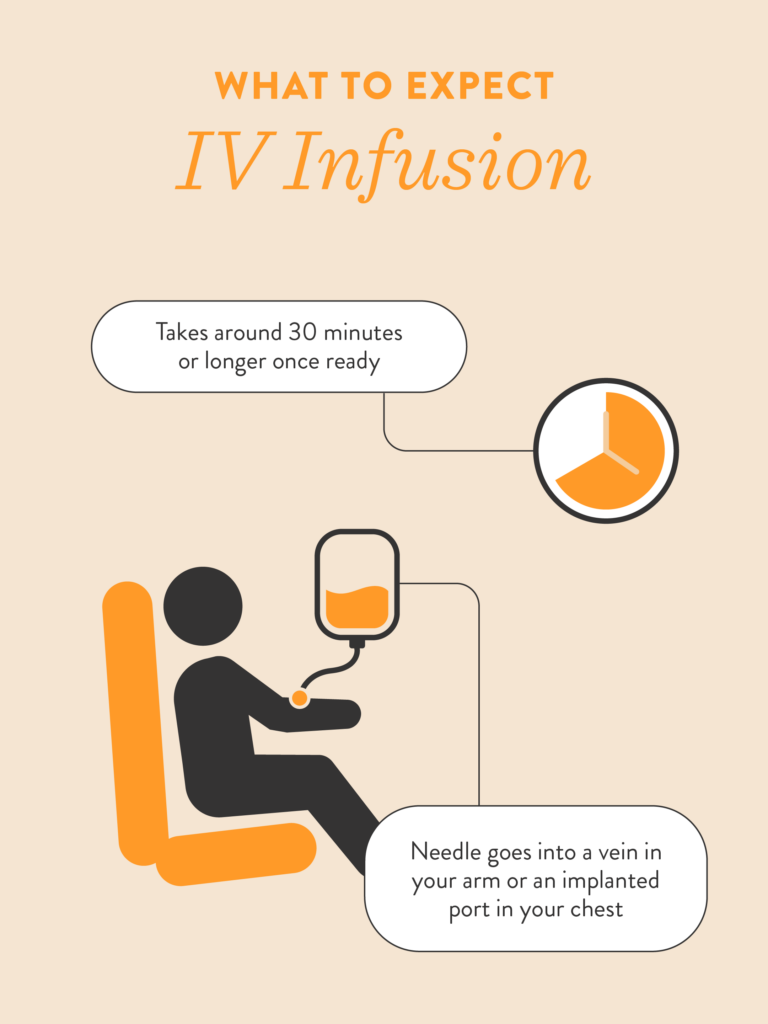
An IV infusion delivers medicine directly into a vein in the arm or through an implanted port in the chest. While both methods deliver the same medicine, IV infusions use a larger amount of fluid and take longer to administer than subcutaneous injections.
3. Does the medicine work the same way?
Yes. Both IV infusions and subcutaneous injections deliver the same immunotherapy medicine, and it works the same way in the body. The main differences are how the medicine is given and how long it takes.
4. How long does a subcutaneous injection take?
Once the medicine is ready, a subcutaneous injection usually takes about 2 to 8 minutes to administer. This is much shorter than an IV infusion, which often takes 30 minutes or longer.

5. Where will I receive my treatment?
Both subcutaneous injections and IV infusions are given at a healthcare facility by trained medical professionals. Even though the injection is quicker, it is still administered in a clinical setting.
6. What happens during a subcutaneous injection?
You will be seated comfortably, and the healthcare professional will access the appropriate injection site, usually the stomach or thigh. They will pinch the skin, insert a needle, and keep it in place for several minutes while the medicine is delivered. Afterward, you are typically observed for a period of time to monitor for side effects.
7. Will the injection hurt?
You may feel some sensation as the medicine is given, but it should not cause significant pain or discomfort. If you feel discomfort or notice a lump under the skin, it’s important to tell the healthcare staff right away.
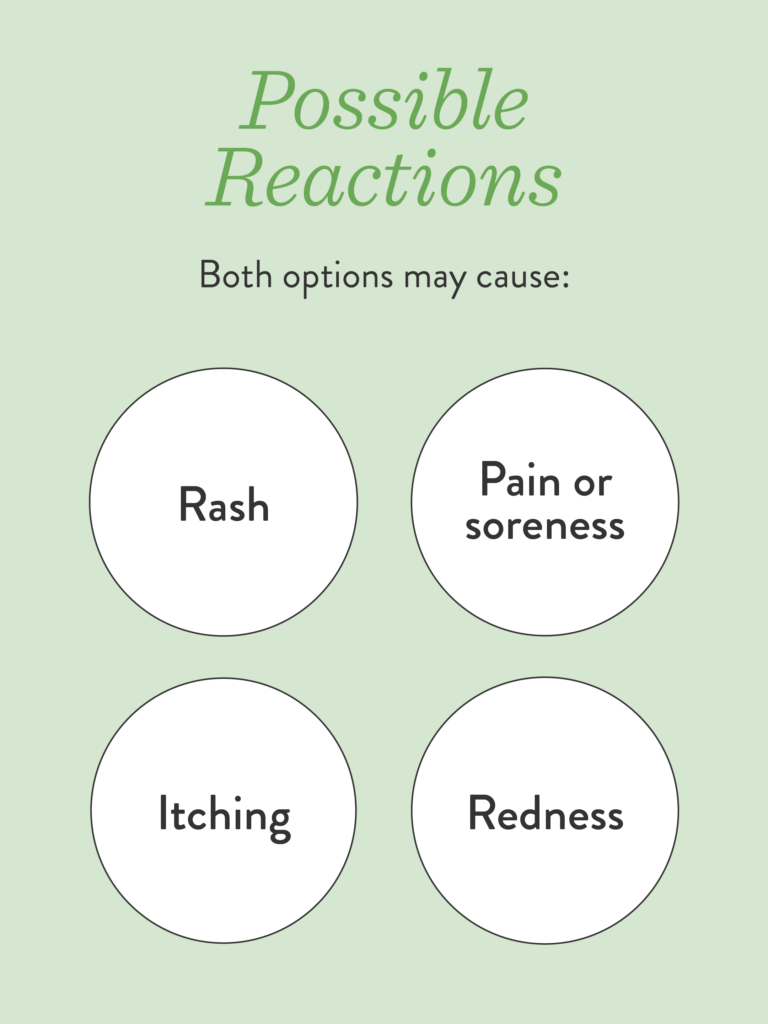
8. What side effects can occur at the injection site?
Some people experience injection-site reactions such as redness, itching, soreness, pain, or a rash. Similar reactions can also happen with IV infusion sites, though the location differs.
9. Can I switch between IV infusion and subcutaneous injection?
In some cases, patients who currently receive immunotherapy by IV infusion may be able to switch to a subcutaneous injection. If subcutaneous injections are not right for you, switching back to IV infusion may also be possible. Your medical oncologist can help determine what option is appropriate.
10. How do I know if a subcutaneous injection is right for me?
There may be medical reasons why a subcutaneous injection is not an option for certain patients. The best next step is to talk with your medical oncologist about your treatment goals, preferences, and any medical considerations to decide which method is best for you.
Thanks to Kristin Bednarz BSN, RN and Daniel Appiah, PharmD, MBA, BCPS, BCOP from Roswell Park Comprehensive Cancer Center for their contributions.