

The Kidney Cancer Association and the Sickle Cell Disease Association of America are partnering to raise awareness about sickle cell trait and its link to renal medullary carcinoma to promote early identification, proper care, and increasing positive outcomes for patients and families.
KNOW your SCT status – Although most people with SCT never experience any symptoms, being aware of your SCT status can help to better treat rare issues when and if they do occur.
KNOW the signs of RMC – If you have SCT, watch for symptoms and push for further evaluation.
TELL family members – Abnormal hemoglobin is inherited, so children and family members of people with SCD and SCT are also at risk.
TELL your doctor – Many doctors still consider SCT a symptom-free condition and may overlook or disregard symptoms that could require special treatment due to your SCT status.
Hemoglobin is the part of a red blood cell that carries oxygen from our lungs to other parts of the body. Normal blood cells are round and soft and contain hemoglobin A. Sickled hemoglobin (hemoglobin S) have a sickled (crescent) shape, are more rigid and become sticky. The sickled blood cells have difficulty passing through small blood vessels and can cause damaging blockages that prevent oxygen and nutrients from getting to certain parts of the body. While blood cells with hemoglobin A will live for 120 days, blood cells with hemoglobin S will only live for about 16 days. This shortened life span causes red blood cell levels to drop, resulting in anemia.
If a person has only hemoglobin S, they have a condition called sickle cell disease (SCD). Anemia and blocked blood vessels cause problems breathing, fatigue, infections, organ and joint pain, strokes, vision problems and spleen issues. Although bone marrow transplants are possible, there is no largely available cure for this condition. There are rare instances where hemoglobin C, D, E, or beta-thalassemia is found instead of hemoglobin S, so it is important to know the exact type of hemoglobin you have.
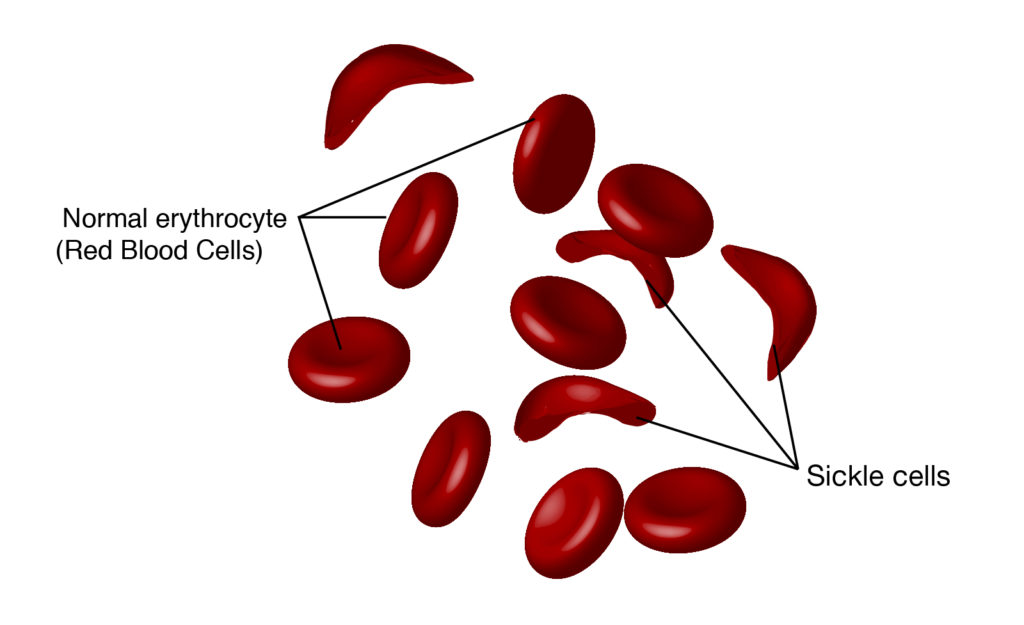
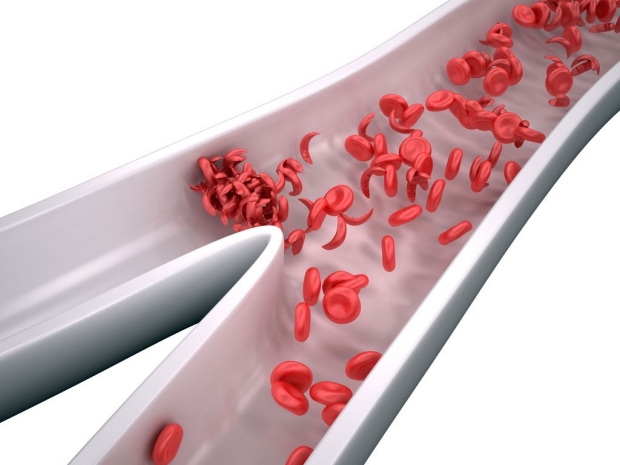
Sickled red blood cells can clump and have difficulty passing through blood vessels to deliver oxygen and nutrients to tissues.
Sickle Cell Trait Rates in the US
| Ethnicity | % born in US with sickle cell trait |
|---|---|
| Caucasian/European | 0.3% |
| Black | 7-10% |
| Hispanic | 2% |
| Asian/Pacific Islander | 0.2% |
Sickle cell trait is particularly common for those with ancestors from Saudi Arabia, India, Mediterranean countries, South America, Caribbean countries, Central America, and sub-Saharan Africa. Adapted from the Centers for Disease Control and Prevention.
On the other hand, people with sickle cell trait (SCT) have some red blood cells with hemoglobin A and some with hemoglobin S. The hemoglobin A helps control the hemoglobin S, so people with SCT are generally healthy and often do not know that they have the trait. People with SCT are not at risk for getting SCD, but they could experience some SCD symptoms when their oxygen intake is limited (e.g., during events of severe dehydration, high altitudes, scuba diving or extremely strenuous exercise).
SCT is more common in some ethnicities than others (Figure 2), however, every newborn in the United States, Canada, and Europe is tested for SCD and SCT regardless of their ethnic background through newborn screening a few days after birth. Despite this widespread screening, test results may not be communicated properly to the family and can be hard to track down later. This means that many people remain unaware of their SCT status and may go their entire life without knowing where they stand. The most accurate way to find out your SCT status is by doing a simple blood test called hemoglobin electrophoresis and complete blood count (CBC) that includes a mean corpuscular volume (MCV).
Renal Medullary Carcinoma (RMC) is a rare but aggressive type of kidney cancer first described in the 1990s1. Approximately 76,000 people will be diagnosed with kidney cancer in the United States in 2021. Despite the increased research into rarer forms of kidney cancer, there are currently no good methods of preventing or detecting RMC in people who do not show symptoms. Unfortunately, these symptoms may not be present early in the disease, making early identification a challenge. Late diagnosis results in higher death rates and shortened life spans, and over 90% of people with RMC have already had the cancer spread to the lymph nodes or other organs by the time they are diagnosed. Studies to improve diagnosis and treatment for RMC are still limited due to how rare it is, and sadly, many of the current therapies used for other kidney cancers do not work well against RMC.
Symptoms
Key statistics
Although the exact reason for the connection is unknown, more than 95% of people with RMC have SCT2. Not all people with SCT will get RMC; in fact, of the 300 million people worldwide with SCT, only 1 in every 30,000 will also be diagnosed with RMC. It should be noted that because RMC can be confused with other kidney cancers such as collecting duct carcinoma, it is possible that the true occurrence of RMC is higher.
The risk for RMC with SCT is low but knowing what to watch for is crucial to detecting it early. If you have SCT and experience any of the symptoms in Figure 3, see a doctor right away and explain your concerns. Studies show many patients experience symptoms for five months before seeking a diagnosis3 which delays possible treatment. When you arrive at the appointment, tell your doctor immediately that you have SCT and inform them of its connection to RMC. One of the key early indicators of RMC is the presence of blood in urine. Your doctor may test your urine to identify particles that can’t be seen by the naked eye. It is important to note that two to three percent of people with SCT have blood in their urine, so your doctor may consider your result normal; however, because this can be an early sign of RMC, people with this result should consider further evaluation. This could include an ultrasound to look for kidney tumors. If tumors are seen, your doctor may want to sample them before you start any other treatments to get an accurate assessment4. Special tests (called immunohistochemistry) can be run on the tumor to confirm an RMC diagnosis. Because RMC is so rare, it is recommended that proper biopsy samples be stored5 and that you get referred to a specialist who has experience in treating this type of cancer before doing anything else6. The earlier the appropriate treatment can be started, the better the outcome – for any cancer patient.
(1) Davis CJ, et al. J Surg Pathol. 1995 Jan; 19(1):1-11.
(2) Elliott A and Bruner E. Arch Pathol Lab Med. 2019; 143:1556-61.
(3) Ivarez O, et al. Pediatr Blood Cancer. 2015 Oct; 62(10):1694-9.
(4) powerfulpatients.org/2020/08/27/what-health-disparities-exist-for-patients-with-renal-medullary-carcinoma.
(5) Msaouel P, et al. Clin Genitourin Cancer. 2019 Feb;17(1):1-6.
(6) Beckerman KE, et al. J Oncol Pract. 2017 Jul;13(7):414-21.
In partnership with the Sickle Cell Disease Association of America
Have questions? Get one-on-one support through the Patient Navigator Program.
Contact [email protected] | 1-800-544-3KCA